Guest blog post.
My name is Eloise Thomas and I live in Perth WA. My ex husband and I found out that we were expecting our first baby in November 2007, just after our first wedding anniversary. We were absolutely thrilled and excitedly anticipated his due date of the 27th July. Throughout my pregnancy I had early pre-eclampsia, very high blood pressure and polyhydramnios. I was hospitalised for the final four weeks of the pregnancy on and off and had two amnio-reductions as I was producing way too much amniotic fluid and there was a chance that bub was having a “blockage of some sort”. We were told that “something was wrong”, but no one could figure out exactly what was wrong because the ultrasounds were showing a healthy baby who was growing well and not showing any signs of distress. I had a CTG every day for the final fortnight and bub wasn’t reaching the levels that were required, so I was booked in to be induced a week later on a Thursday.
Charles William Thomas (Charlie) was born just before 6am that morning by emergency c-section. My waters broke naturally at 2am and there was so much amniotic fluid, I felt like my organs were falling out. It was frightening to see that much fluid coming out of oneself (too much information, sorry). I think I even apologised to the midwives, who found that rather amusing as “it is what we do everyday” was their answer. I will never forget seeing our beautiful tiny little boy for the first time. He was brought up to my face so that I could see him and rub cheeks with him, but before I knew it he was rushed out of the room and the rest is rather foggy.
My ex-husband was absolutely amazing and went through so much while I was ‘fuzzy’ from the epidural and all of the other medication that I was on. All I remember from that day is being wheeled into recovery and immediately calling my parents and sister to share the news and to SMS every other person in my phone to tell them our joyous news. I had no idea what was ahead. I remember waking up a few hours later in my private hospital room when Charlie was brought in. He was attached to all sorts of different tubes, was lying on his stomach and inside a huge humidi-crib. He had at least five people around him, two of whom were Doctor’s, and they were rushing him straight to Princess Margaret Hospital where he required emergency surgery. I found out later that this was my opportunity to say ‘goodbye’ to him if the surgery was not to be successful. I don’t remember much of this, only what my ex-husband told me.
I have never been a Mum before and didn’t know what ‘normally’ happened after you have a baby.....did your baby stay with you? I’m sure that is what happened. Are all babies taken away for a while? I did know that something wasn’t right from the beginning but everyone was keeping me informed on a ‘need to know’ basis, rather than provided me with all of the information that perhaps I wasn’t ready to receive right there and then.
Charlie born full term with Tracheo Oesophageal Fistula (TOF)
Our Charlie was born a TOF baby. He has Tracheo Oesophageal Fistula, where his trachea and oesophagus were joined and leading to his lungs, so he had no tube going to his stomach and he could not swallow (this explained the excess amniotic fluid) and he had breathing difficulties. My little angel was rushed to the children’s hospital only a few hours after he was born. I saw him four days later. He was kept in the Neonatal Intensive Care Unit at PMH for his first ten days and we will never forget that time. A frightening time where we had no one there to support us and let us know that yes, our journey was a difficult one and that it was normal for us to be feeling like we were drowning and so completely helpless. It was a very lonely feeling for the both of us.
Charlie was tube fed for the first ten days of his life, so feeding was a huge obstacle that took a long time and getting him used to bottle feeding was a huge challenge. Breast feeding was too distressing for the both of us, so after much painful deliberation, I chose to put him on formula. He also had severe reflux, so required a thickened feed. I begged my OB to discharge me from the hospital ASAP and we went to live in the parents quarters at the NICU to be close to our boy. I was called into the NICU every three hours to feed him, express my milk and then return to the parents wing to catch up on some sleep, all while in agony due to getting an infection in my caesarian scar. My body didn’t respond well to anything at this time. Every day I could watch him, touch him but could not hold him. He had so many tubes attached to him, it took one of the NICU nurses about 20 minutes just to change his nappy. He was so small and sickly looking. It was very surreal.
After 6 days his wires were slowly coming off, we were trying to establish feeding and we were able to hold him for the first time. What an occasion that was. One that I will never forget. After the 10th day, Charlie was transferred back to the original hospital where I had him (SJOG Subiaco) where he remained in the Special Care Nursery under close watch until we could establish feeding. I hired the Mothercraft room, right across from the SCN where I learned how to look after him and feed him, under the close watch and assistance of the amazing staff there. And after three weeks, we were allowed to go home.
From when we got home to when Charlie was five months old, we nearly lost him nine times due to ‘death spells’ where his trachea would collapse (due to feeding/crying and the normal things babies do). I was too afraid to put him for sleeps in his bassinet, so he would sleep on my chest during the day and we had him attached to a monitor for him to sleep in our room during the night. We couldn’t let him cry, otherwise he’d get distressed and have an ‘episode’ where he would struggle for breath and go blue. We had him attached to the heart monitor then at all times and had oxygen tanks on standby in case he required some help. We had eight hospital stays in this time, so that his medical team could monitor him. I couldn’t count the number of doctors, nurses, specialists etc that we saw and each was equally surprised when they saw his hospital ‘portfolio’ because it seemed to always be the thickest in the pile for a child so young.
Charlie was put onto reflux medication and his feeds were thickened more, which helped a lot. He had regular appointments every month so that his medical team could keep a close eye on him and we still have yearly appointments with his team and he turns 6 next month. He has had appointments for surgical, neonatal general, monitoring, speech pathology, audiology, palette (he has a sub mucus cleft palate and a double uvula), physiotherapist and respiratory. He only had two dilatations (incredibly fortunate for a TOF kid), where they insert a rubber knitting-needle type object, dipped in oil and put down his throat right down into his tummy to ensure that the oesophagus remains stretched and open, to prevent any obstructions to add to his swallowing difficulties.
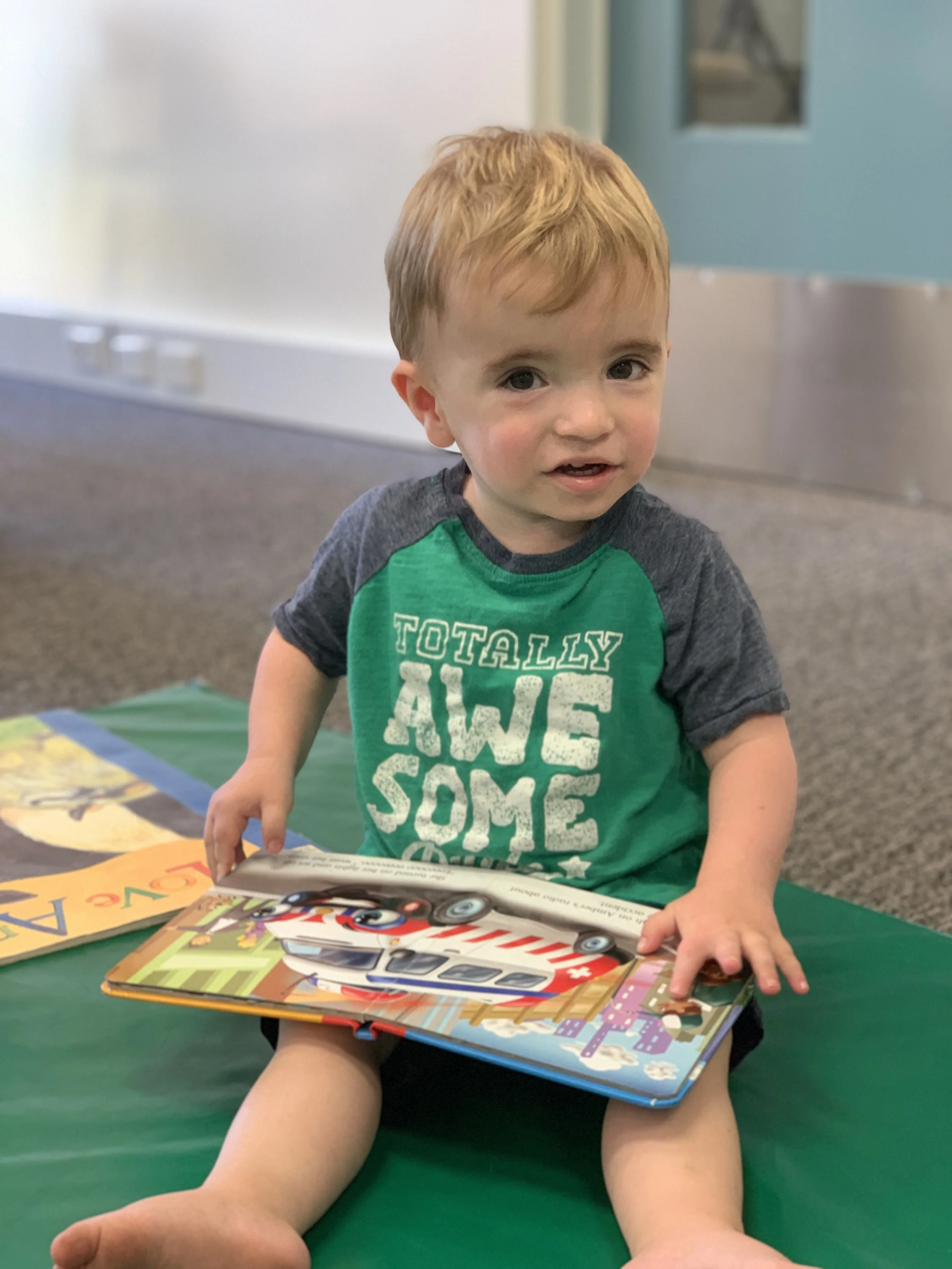
He wasn’t able to eat normal foods for a long time as his oesophagus was not as ‘coordinated’ as it should be, so he was on mashed up food for a long time and I may have done a happy dance in Coles when he was able to eat his first Milk Arrowroot bicky at 2 without choking. And we have been on a steady road ever since. His last episode was two years ago and Charlie is now a robust, strong and fast growing little boy who turns 6 next month. He has had no other health issues, is eating me out of house and home and loves school. After such a rough start, he has really shown us how amazing he is and we are so incredibly proud of him.
You may also be interested in these stories :